Researchers have developed an experimental therapy using engineered neurons derived from stem cells that effectively “soak up” pain signals before they reach the brain. Initial tests in mice with arthritic knees suggest this approach could offer a new way to manage chronic pain, potentially reducing reliance on opioid medications.
The Mechanism: A Biological Decoy
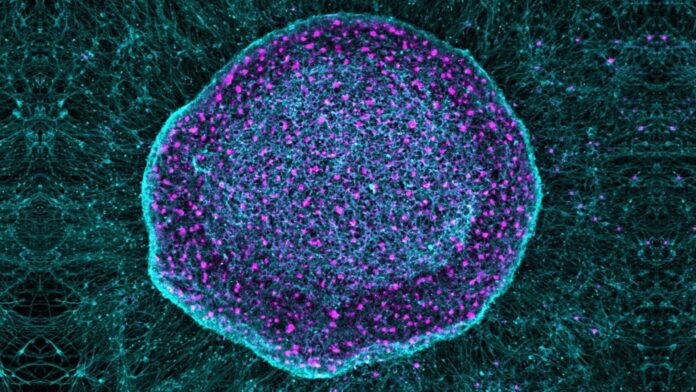
The therapy, dubbed SN101, utilizes human pluripotent stem cells (hPSCs) – cells capable of becoming any cell type in the body. Researchers, led by Gabsang Lee at Johns Hopkins, engineered these hPSCs to differentiate into specialized sensory neurons. These neurons act as a biological “sponge,” intercepting inflammatory pain signals at the site of inflammation before they can be transmitted to the brain.
This differs from current pain management strategies. Opioids work by blocking pain signals in the brain, essentially masking the sensation. SN101, however, targets the source of the pain by sequestering inflammatory factors. The engineered neurons bind to these factors, preventing the body’s natural pain-sensing neurons from detecting them.
Osteoarthritis and Beyond
The study focused on osteoarthritis, a common degenerative joint condition that causes chronic pain and inflammation. However, the researchers believe the therapy could theoretically work for any type of chronic pain. Osteoarthritis itself affects millions, causing joint breakdown and no known cure. Current treatments involve lifestyle changes, painkillers (including opioids), and steroid injections—all with significant limitations.
The engineered neurons also demonstrated an unexpected benefit: promoting cartilage and bone repair in the mice. This dual effect – pain relief and potential tissue regeneration – is particularly compelling for osteoarthritis, where cartilage degradation is a primary issue.
The Opioid Crisis and Safer Alternatives
Chronic pain is often treated with opioids, which carry risks of addiction and unwanted side effects. Roughly 9% of patients with knee osteoarthritis turn to opioids, sometimes long-term. This drives the search for safer and more effective alternatives. SN101 may offer a more biologically attuned approach by mimicking the body’s own pain signaling system.
Remaining Hurdles
Despite promising results, SN101 remains preclinical. Significant challenges remain before human trials can begin:
- Immunogenicity: Ensuring the engineered neurons don’t trigger a harmful immune response is critical.
- Translation to Humans: Mouse joints differ substantially from human joints, and pain processing varies between species. Long-term safety assessments and toxicology studies are essential.
- Scale and Durability: Human joints are larger, more complex, and subject to decades of stress, which may impact efficacy.
As Yale orthopedics professor Chuan-Ju Liu notes, the idea behind SN101 is “innovative,” but rigorous testing is required. This includes formal toxicology studies, long-term safety assessments, and first-in-human clinical trials.
The research is still in its early stages, but the potential to relieve pain without the risks of opioids while simultaneously promoting tissue repair makes this a compelling area of investigation.
The long-term viability and safety of SN101 remain uncertain, but the approach represents a significant departure from traditional pain management and offers a glimpse into a future where chronic pain might be treated at its biological root.